Welcome!
Thank you for reading the November 2020 edition of the Magnet® Newsletter from Tipton Health Communications. This edition features firsthand accounts from nurses across the country who have been fighting against COVID-19, how to incorporate your nurse’s stories into your Magnet documents, and other tips and insight from the experts at Tipton Health Communications.
Article Navigation
- COVID-19 Warriors – The Forefront of True Grit and Resilience
- What is Your Warm Blanket?
- Maintaining Magnet in the Midst of COVID-19
- Finding the Silver Lining
- You Give Me Hope
- From the Front Lines To the Page – Incorporating COVID-19 Stories Into Your Magnet Application

Thank you for joining us for this very special edition of the Tipton Health Magnet Newsletter. We turn this issue over to you — the courageous and wonderful nurses who have literally put their lives on the line to care for others during the COVID-19 pandemic.
Remembering these stories of bravery, innovation, leadership and every day commitment is important. We have created a special website at www.nurseherostories.com to record and share your stories.
We encourage you to post your personal remembrances. What was your worst day and what got you through it? What examples of empowered nurses did you see? How were you and your leadership team transformational?
Following are just a few of your remarkable stories. Be sure to register to hear nurses tell their stories during our special Nurse Hero Stories webinar on November 10th at 12:30 EST.
COVID-19 Warriors: The Forefront of True Grit and Resilience
Marifel (Max) Axalan, BSN, RN, CNN, Nurse Clinician – NewYork-Presbyterian Hospital/Weill Cornell Medical Center

As I sat down and contemplated my unit’s experience during the pandemic, I was suddenly overwhelmed with emotions. My throat was tight, my eyes were blurry, and the tears just kept falling. “I survived COVID-19! My teammates survived COVID-19!” I could hear my brain screaming over and over, “This is victory!” Or is it?
It was March 16 when N2/N8 Hemodialysis and Apheresis nurses were finally called into action: Dialyze COVID-19-positive patients. Our patients need us. We were physically at our patients’ bedside for over four hours straight from beginning to end of dialysis treatments. We endured the profuse sweating under our PPE (like having continuous “hot flashes”). We didn’t dare leave our patients’ side for bathroom breaks so we held the urge until the treatments were done. In those fearful moments, we knew we were extremely exposed and vulnerable to this unknown enemy. But we were all determined to fight it with all our might. We had to win this battle for our patients, for our families, and for each other. Our team became more cohesive than ever. We shared each other’s strategies on how best to protect ourselves. We wore impermeable blue isolation gowns, we used face shields, N95 masks, surgical masks, shoe covers, bonnets, anything available—we had them on. Endless hand-washing and disinfecting. Without a doubt, our infection control practices were above and beyond! Our staff bathroom was even outfitted with a shower we could use at the end of our shifts. It felt like we washed away some of the fears at bringing the enemy home to our loved ones. But in that tiny corner of our hearts, the dread and uncertainty lingered.
We were so thankful to have had the immense support of our empowered department and NewYork-Presbyterian leaders; the dedication demonstrated by our equally committed partners (Medical Director, Nephrology Team, and Hemodialysis Technicians); and lastly our hardworking NewYork-Presbyterian/Weill Cornell colleagues, associates, and support staff. Indeed, our mission was made possible by the unsurpassed generosity of our institution to provide us the supplies and equipment we desperately needed while other institutions were found lacking. Not to mention the bountiful nourishment, free accommodations and transportation, laundered scrubs, financial and mental health support, and so much more. Indeed, all these provisions and resources kept us going. Somehow, the heavy burden became bearable. We were beyond grateful.
The trials and tribulations came in droves. Our patients were acutely sick and we never knew when the next time we would see them would be. Our goodbyes seemed more frequent. But there was one goodbye we never imagined saying…to one of our own. Our hearts were broken. Our resilience wavered, and our spirit—almost defeated. She was a fearless warrior. An extraordinary nurse who possessed unrivaled grit and valor. We missed her dearly and found comfort amongst each other. Emotional support poured in even from strangers.
In the midst of all this unimaginable devastation and anguish, our faith was our lifeline. It held us steadfast. Prayers were our constant companion and ally, our infinite source of strength. We filled our minds with positive thoughts to rebuild our spiritual defenses. Our heart-to-heart virtual or phone conversations with families and friends and near others strengthened our grip on our daily emotional struggles. Our nutritious dietary intake and the fanatical regimen of doses of vitamin C, prebiotics, probiotics, and other immune-boosting supplements kept our physical defenses almost impenetrable.
Looking back, the whole experience seemed surreal. And so here we are—heart in pieces, bruised faces, battered spirits, but still standing strong and hopeful. Our Hemodialysis/Apheresis Unit even won 2020 Weill Cornell’s much coveted Structural Empowerment Award. Truly, we are all in this together. Without a doubt, this is victory.
Sign up to hear more nurses tell their stories in our upcoming webinar.
Top of Page
What is Your Warm Blanket?
Kari-Lynn Malec, RN, Interventional Radiology at Henry Ford Hospital
What is your warm blanket? A nurse collecting unemployment during a COVID crisis, a global healthcare pandemic? Who thought this could happen? An RN was redeployed from a navigator position to ED to home care and eventually to taking a personal leave and then a furlough. Wow! How did this happen? How come I couldn’t go? Every day upon arrival at work I asked to be redeployed. I was not sent. Thirty-one years of experience, a graduate degree, a national certification and a plethora of experience. Wanting to support the true hero—the nurse at the COVID patient’s bedside. The hero nurse—I sure didn’t feel like a hero. The media told me I was one. My neighbors dropped off gifts, leaving them on the front porch. They were supporting the hero. I was not. I was sitting home guilt-ridden because I was not at the bedside.
The development of a basic concept of nursing emerged. I could not find my warm blanket to hand out or a pillow to fluff. Reflecting on my position and wondering what the warm blanket I was providing was, as I was not supporting my colleagues, nor did I feel I was contributing like a hero. I was looking inward when I needed to be looking at finding a place back at the bedside where I could put a warm blanket on someone. I sunk to a dark place with no self-worth and felt for the first time in my career no one wanted me. I didn’t feel like a hero. I didn’t feel like a real nurse.
My colleagues were struggling around the country as I sat and did my office job. I didn’t know where my warm blanket was. Often, my thoughts would drift to bedside patient care. How could I change jobs in the midst of a crisis when nurses were furloughed? Knowing the crisis could come back in the fall and winter and being in the same position again but wondering whether I would be paid this time. It all came down to the general concept of the warm blanket. Maybe I couldn’t support my colleagues, but maybe I could go somewhere where I could be with the patient. I needed to change my focus on how or when to apply the blanket. I needed to suppress the guilt or release it. I always wanted to teach a class on giving love—fluffing a pillow, putting a warm blanket on a patient and tucking them in—not innate in some people.
People learning with the overwhelming nature of academia have a difficult time applying concepts and “giving love.” It is significant to look in a patient’s eyes and share the love. Supporting, guiding—and the true nature of our calling to nursing. The education to support the practice, and the love to help guide the patient through their journey. As an ED nurse for many years, recognizing that an injured toe or a GSW is still a journey for that patient. And everyone can close their eyes and feel the nurse through the application of a warm blanket. My thoughts continuously flowed to the bedside. Holding a hand, fluffing a pillow. Helping guide a patient through their journey while I am at the bedside. This is my true calling. This is where I belong and where I can support my colleagues. I don’t need to be a hero. I just need to hold the warm blanket for when it is ready to be applied.
What is your warm blanket?
Sign up to hear more nurses tell their stories in our upcoming webinar.
Top of Page
Maintaining Magnet in the Midst of COVID-19
Madelyn Torakis, MSN, RN, NE-BC, Director, Nursing Excellence and Magnet Program – Henry Ford Hospital
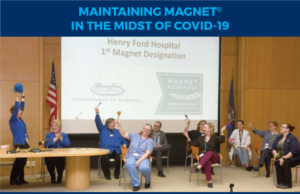
September 23, 2013. My first day as an employee of Henry Ford Hospital (HFH). I was hired into this amazing organization to help lead the efforts to achieve Magnet® designation, the highest honor and recognition for nursing excellence in the world. I worked hand in hand with Gwen Gnam, Chief Nursing Officer and VP Patient Care Services, on this journey. We built programs from the ground up, revised existing programs and reinforced a culture of excellence, autonomy and pride amongst our nursing staff. Finally, in February 2019, we submitted all the supporting documents to the Magnet Recognition Program for review by a team of appraisers. We waited for a response, submitted additional clarification documents and waited some more. The next step in the process involved a site visit by the appraiser team, which we were finally granted in January 2020. It was an amazing three days! The appraisers were wowed with everyone they spoke with—nurses, physicians, support staff. All this took place before we even thought about or even really heard about the coronavirus. Although it was only a few short months ago, it feels like it was in another lifetime.
After the site visit, we waited again, this time to receive a call from the Magnet office informing us that the Commission on Magnet Recognition wanted to call us publicly to announce their decision. That call came to us on Thursday, March 12. We arranged for our official call to take place on Friday, March 20, at 9:15 a.m. We were understanding more about the coronavirus by this point and the guidelines indicated gatherings of no more than 250 people. We had dreamed of this day for 6½ years and we knew that the Buerki auditorium could easily accommodate that number of people. After all, we had planned a big celebration! By Monday, March 16, however, gatherings of 250 people or less was changed to 50 people or less, and by Wednesday, March 18, it was down to no more than 10! We decided that the coronavirus was not going to rob us of our joy, so we gathered 10 of us on the stage in the Buerki (maintaining social distancing), invited people to join us on the conference call and live-streamed it on the SONIFI TVs on the units. We received the great news we had hoped for and the 10 of us celebrated as if there were 100 of us in the room! We were finally being recognized as a Magnet hospital—something we had known we were all along!
Very quickly after our designation call, HFH went into full COVID-19 survival mode. It has been challenging to say the least, but I can honestly say that we have proven over and over again why we are a Magnet hospital. Leadership, teamwork, resiliency, advocacy, autonomy, compassion, innovation, dedication and tenacity. These are only some of the words to describe the culture of Henry Ford Hospital. We know that together we will make it through to the other side of this. And when we do, there will be much to celebrate (with a gathering of more than 250 people)!
A note from one of the Magnet appraisers:
“You all have been in my thoughts especially as I see all the stories of what HFH is facing during this pandemic and all that you are doing to care for the people of Detroit. It was an honor and a privilege to visit your organization and I am so happy for all of you. My very best wishes to you, Gwen, Ronnie and all the fabulous nurses at HFH.”
Click here to hear Madelyn tell her story firsthand.
Sign up to hear more nurses tell their stories in our upcoming webinar.
Top of Page
Finding the Silver Lining
Jeanie Hubert, OR RN – Hunterdon Medical Center
![]()
COVID-19 had a silver lining for me because it allowed me to use my skills as a medical-surgical nurse to care forothers when it was desperately needed. I have been an operating room nurse for the last four years; however, I have a background in medical-surgical nursing. In the coming of the COVID-19 pandemic, I decided to put my “med-surg nurse hat” back on and put my skill set to good use.
During the months of March, April, and May, I was redeployed as an emergency room nurse at Hunterdon Medical Center. I was able to use my skills in medical-surgical nursing that I do not normally employ on a daily basis in the operating room. Jeanie the med-surg nurse was back in full force; in the blink of an eye, I was starting IVs, drawing bloodwork, administering various medications and treatments, and performing numerous bedside procedures in an emergency room that was overwhelmed with patients. The emergency room never slowed down during the 12-hour shifts that I worked. The other (incredible) nurses and I gave our all to these patients; we worked in sixth gear from the minute that we arrived to the minute that we were able to go home. We were absolutely exhausted at the end of each day.
In addition to serving in the ER, I worked at pop-up field hospitals just outside New York City. These hospitals were rapidly constructed by the U.S. military. Patient rooms were merely cots that were separated by curtains. Six large oxygen tanks fed each patient “wing,” with oxygen tubing running directly to each individual room. One medication cart supplied each wing. It was like the television show M*A*S*H came to real life in 2020. I truly felt like I was in a movie of some kind. I worked 12- to 14-hour shifts straight through—not taking any breaks to eat, drink, or use the bathroom because I did not want to remove my mask (or my hazmat suit). I averaged about 70 hours per week, caring for patients infected with COVID-19. Almost daily I watched patients die from respiratory failure, despite our best efforts to recover them. I watched the patients rapidly deteriorate right in front of me. I cared for patients of all ages; some as young as their early 20s were unable to maintain their oxygen saturation above 90% without supplemental oxygen. It was the most horrific experience in the seven years that I have been a nurse, without a doubt.
I am thankful for the experiences that I had as a professional; however, I am deeply saddened by the impact of COVID-19. Many patients did not survive, and my heart is heavy with grief for those we could not save. This experience was life-changing; I appreciate the simple things in life—like a “typical day at work” or a bright and sunny day—on a whole new level.
Sign up to hear more nurses tell their stories in our upcoming webinar.
Top of Page
You Give Me Hope
Lorraine Lewis, BSN, RN, originally from Cardiac Cath Lab – Long Island Jewish Medical Center
![]()
With the rapid closure of the Cardiac Cath Lab, Lorraine volunteered to be redeployed to the Emergency Department (ED). She chose the ED because of both her clinical background and familiarity with the Senior Admin Director, Helena Willis, MSN, RN, CEN. She and Helena had worked together in the past and maintained a relationship. Lorraine worked mostly in the “tent” and was immediately impressed by the level of support and comradery there.
The support from and for each other was amazing. She acknowledged that everyone was scared to death, the unknowns of this virus were overwhelming, but “we all hung in together.” When the ED volume started to drop, the tent closed and then Lorraine just volunteered to work in the MICU that was created in our Interventional Recovery Suite (IRS).
Lorraine was fortunate to be with a coworker, Marykate Alcusky, BSN, RN, CEN, in the ED. When their services were no longer needed there, together they went to the MICU annex located in the IRS. Again, Lorraine was amazed by the comradery and the support they received from the nurses in the area. Most notable to Lorraine was one of the agency nurses. She felt that the agency nurses would be “guests in our home” and quickly realized that indeed they became family as well. One particular nurse, Ashley, left a special mark on Lorraine.
Ashley is a travel nurse originally from Florida. She joined the MICU staff and was often working in the IRS. Lorraine was immediately taken by Ashley’s incredible bedside manner. Lorraine recalled visiting a patient that Ashley was caring for. Lorraine had a bond with the family and tried to visit whenever she could. On this day, very shortly after Lorraine arrived, this patient, “Juan,” began to desat and become significantly bradycardic, Ashley jumped out of her seat before Lorraine could say a word. Ashley’s comment, “No one dies alone here,” and the fact that she ran into the room to hold his hand will be forever etched in Lorraine’s memory.
Lorraine spoke of the need for humanism and human touch. She felt the pictures and anecdotes posted around the room about the patient and the family helped to develop relationships. It was difficult, particularly in Surge B, because the environment could easily be overwhelming. When asked about support from management, both from her home unit and the new units, Lorraine enthusiastically replied that she felt supported. Units worked as well as they could and she was comfortable knowing that she was part of the solution. The level of support for each other was amazing! There were no titles, no hierarchy. Everyone chipped in with everything they had. In terms of self-care, Lorraine noted how grateful she was to be working with Marykate in both areas. They would talk every day; on her days off she would have Marykate check on her patients and vice versa. There were times each cried, but luckily they were different times.
When asked about the silver lining, Lorraine spoke of how lucky she was “to meet all these amazing people that I ordinarily would not cross paths with. It was also important to capture any small miracles along the way. Words cannot describe the support I felt from everyone.” Lorraine is also passionate about the fact that, in her eyes, the true heroes are the patients and their families. “We are doing our job, they were fighting every step of the way.” Lorraine states that her strong faith was vital to getting through the past few months. She remembers working with a patient in Surge B who was extubated. She whispered in the patient’s ear, “Thank you. You give me hope.”
Sign up to hear more nurses tell their stories in our upcoming webinar.
Top of Page
From the Front Lines to the Page – Incorporating COVID-19 Stories Into Your Magnet Application
Moira Owens, Senior Editor, Writing Support at Tipton Health Communications

It’s hard to think of a topic that has been more all-consuming than the ongoing COVID-19 pandemic. Since the stories in your Magnet application should represent the spectrum of experiences in your four-year Magnet window, it stands to reason that the coronavirus will figure into one or more of your examples. Learn more about how to do it below.
TL4: Provide one example, with supporting evidence, of the CNO’s leadership that led to a strategic organizational change.
In TL4, you’re asked to write a story about an initiative your chief nursing officer (CNO) led that had an organization-wide impact (meaning it extended beyond the Nursing department). We’ve seen several stories from our clients in which the CNO has led projects related to COVID-19 to ensure the safety of staff, patients and visitors, such as creating comprehensive employee screening, testing and surveillance protocols or centralizing and enhancing personal protective equipment. One CNO opened a “tranquility tent,” staffed by a wellness liaison, a counselor from the Employee Assistance Program, a greeter and a social worker. Hospital personnel can go to the tent when they need a calming space to recharge. There, they can speak with a chaplain or behavioral health specialist. They can find materials to help with meditation exercises. And they can leave supportive notes for one another at specified drop-off spots. Efforts like these can give a huge boost to staff morale.
To write your TL4, remember to use your hospital’s strategic plan (not the Nursing strategic plan) as the anchor to your story, which should illustrate how your CNO’s actions aligned with one of your strategic goals. The rest of your evidence should demonstrate your CNO in action—show by emails and meeting minutes how she or he advocated for the initiative.
There are lots of opportunities for your other nurses to shine in your application. EP13 (nurses applying available resources to address ethical issues related to clinical practice), EP14 (clinical nurse[s] resolving a security issue by making contributions to an interprofessional group) and NK3 (clinical nurses using evidence-based practices that are new to the organization or a revision of an existing practice) are all ways to highlight your nurses’ efforts.
For your Empirical Outcome documents, be sure to report an outcome measure (not a process measure!). Potential COVID-19 outcome measures are average length of stay (ALOS), ventilator-associated pneumonia (VAP) rate or mortality rate.
Here at Tipton, we’ve been overwhelmed with stories that illustrate the heroism, humanity and humility that nurses across the country have demonstrated during these difficult times. Phone us at (302) 454-7901 and find out how we can help you tell your story.
Top of Page
Read More Moving Narratives
These brave nurses’ stories are just the beginning. Read more about how nurses across the country found hope and strength during the pandemic.
Hear Their Stories Firsthand
On November 10th, six brave nurses will re-tell their moving experiences on a live webinar. Please join us to hear their stories.

