
We are excited to announce that Tipton Health is now offering the opportunity to disseminate research studies externally through our Nursing Connections newsletter!
This is an opportunity to share research study abstracts, posters, links to the full research write up (if available), and even to use our publication as evidence in your NK4 example for disseminating a research study externally!
If you are interested in this opportunity, ensure that you get approval from your director or chief nursing officer to provide your research abstract. We will then send you a template including the information we’ll need for publication and how to structure the abstract.
Qualifying for NK4 Submission
If you wish to use this publication as evidence in an NK4 submission, be sure that at least one clinical nurse is listed as a study author and that the submission includes the title of the study, the IRB approval dates, and the study start and completion dates. In your NK4 example, be sure to include the title of the publication and the publication date.
We are proud to present our first external dissemination of a research study from White Plains Hospital below, detailing a qualitative study on the care transition experience of COPD patients over the age of 65 below.
Research Study Abstract – White Plains Hospital
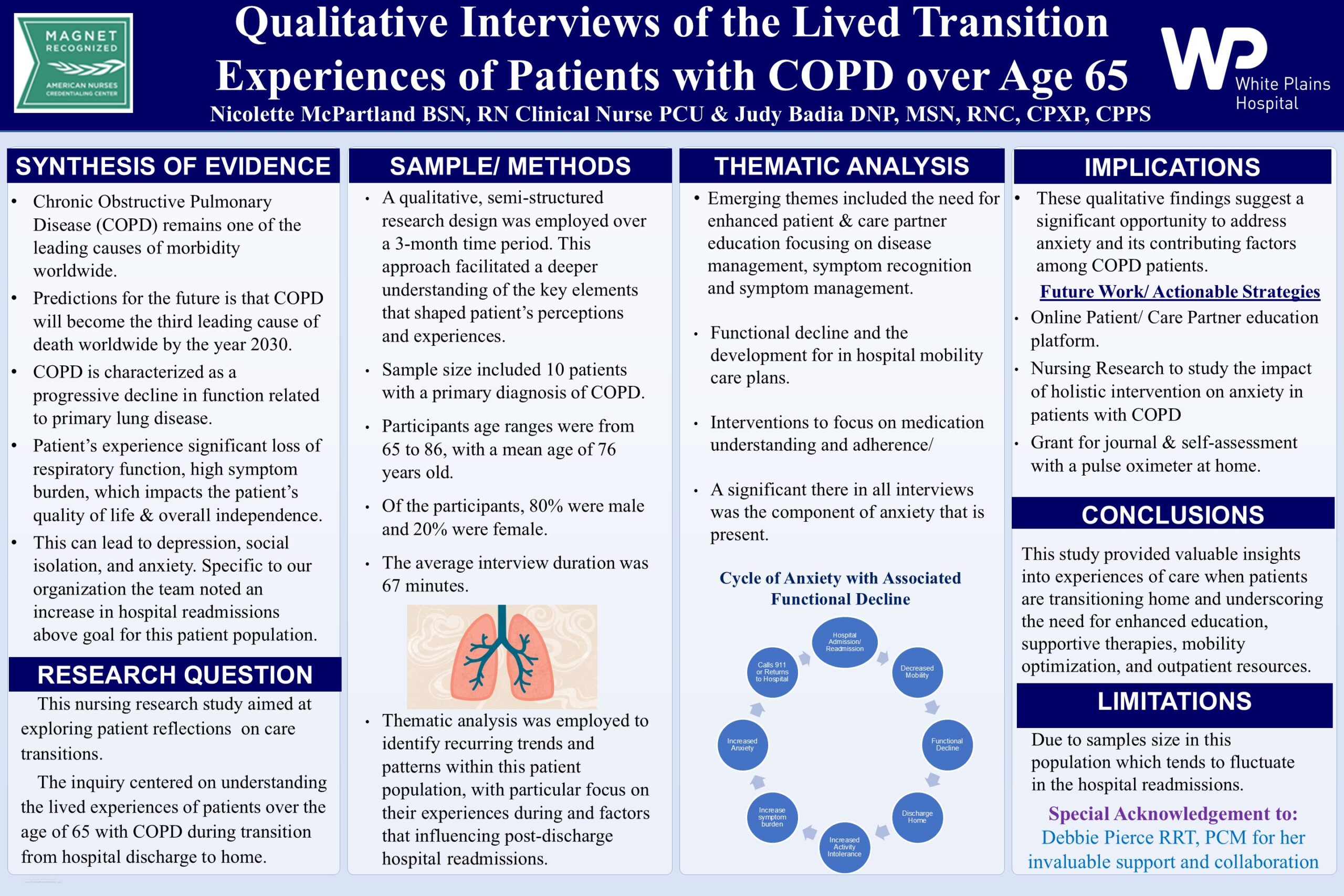 Qualitative Interviews of the Lived Care Transition Experiences of Patients with COPD over the Age of 65
Qualitative Interviews of the Lived Care Transition Experiences of Patients with COPD over the Age of 65
IRB Approval: May 7, 2024
Study Start Date: May 13, 2024
Study Completion Date: December 18, 2024
Investigators:
- Judy Badia, DNP, MSN, RNC, CPXP, CPPS, Clinical Nurse Scientist, White Plains Hospital, White Plains, NY
- Nicolette Mcpartland, BSN, RN, Clinical Nurse PCU, White Plains Hospital, White Plains, NY
- Debbie Pierce, RRT, PCM, COPD Transitional Care Manager, Respiratory Therapy Department, White Plains Hospital, White Plains, NY
Categories of Research: Pulmonary Diseases
Keywords: COPD, Readmission, Functional Decline, Mobility, Education, Discharge, Anxiety
Abstract
Background: Chronic obstructive pulmonary disease (COPD) is the third leading cause of death with those diagnoses expected to rise, creating a substantial burden. COPD management is complex, often involving comorbidities, fluctuating symptoms, and the need for long-term care. The disease significantly impacts a patient’s quality of life, imposing a considerable symptom burden, both physiologically and psychologically. COPD also comes with a financial burden due to treatment costs and quality of life issues for the family or care partner. The purpose of this study was to explore patient perceptions of lived transition in care experiences and gather insights to help health care teams improve care transitions in this population.
Method: A semi-structured qualitative design was employed, involving 10 patients with COPD over the age of 65.
Results: A thematic analysis was conducted that revealed a prominent theme of persistent anxiety among patients diagnosed with COPD, particularly during discharge transitions. Participants expressed feelings of security while hospitalized, comforted by the health care team’s monitoring. Upon discharge, anxiety increased due to fears of leaving the hospital and uncertainties about managing their condition at home.
Anxiety was further compounded by the complexity of COPD, as many struggled with understanding the disease and its progression. They voiced concerns about managing daily tasks like meal planning, medication, and personal care. Financial stress, particularly regarding medication costs, contributed to anxiety, with some altering their medication usage to reduce expenses, risking their health outcomes.
Participants also emphasized the need for better education on managing their condition, especially regarding environmental triggers like weather changes or illness. The lack of understanding from family and friends, coupled with social isolation, added to their stress. Participants advocated for self-monitoring and symptom evaluation, stressing the importance of including this in discharge education to improve disease management and reduce hospital readmissions.
Conclusions: The qualitative interviews reveal the significant impact of anxiety on patients with COPD, particularly during transitions from hospitalization to home. The fear of managing their condition, combined with a lack of understanding and support, exacerbates feelings of stress and uncertainty. Participants emphasized the need for comprehensive education for both patients and their families to improve disease management and outcomes. Key strategies, such as self-monitoring and individualized discharge plans, are crucial in empowering patients to manage their health and reduce readmission risks. Addressing these concerns through targeted support, education, and improved communication could alleviate anxiety, enhance quality of life, and promote better disease management.
Building on these findings, a study is under IRB review that aims to explore the impact of a holistic approach to managing anxiety in COPD patients. Efforts are also underway to enhance online educational resources for patients, families, and caregivers, focusing on critical aspects of COPD management. Additionally, nursing staff training has been expanded, including updated inhaler use instructions and physical therapy materials in COPD patient care protocols. These initiatives aim to improve patient self-management, empower families, and enhance the overall management of COPD.
References:
Aranburu-Imatz, A., López-Carrasco, J. C., Moreno-Luque, A., Jiménez-Pastor, J. M., Valverde-León, M. D. R., Rodríguez-Cortés, F. J., Arévalo-Buitrago, P., López-Soto, P. J., & Morales-Cané, I. (2022). Nurse-led interventions in Chronic Obstructive Pulmonary Disease patients: A systematic review and meta-analysis. International Journal of Environmental Research and Public Health, 19(15), 9101. https://doi.org/10.3390/ijerph19159101
Yawn, B. P., Mintz, M. L., & Doherty, D. E. (2021). GOLD in practice: Chronic Obstructive Pulmonary Disease treatment and management in the primary care setting. International Journal of Chronic Obstructive Pulmonary Disease, 16, 289–299. https://doi.org/10.2147/COPD.S222664
Mail Correspondence to:
Judy Badia, DNP, MSN, RNC, CPXP, CPPS
41 East Post Road
White Plains, New York 10601
Email: jubadia@wphospital.org
914-849-3295
This study did not receive grant funding.
CURRENT ISSUE
PAST ISSUES
Let Us Know How We Are Doing and How We Can Better Support You.
We are absolutely dedicated to your success. We form deep partnerships with our clients based on trust. That requires continuous conversation. Tell us how we can better serve you.
